Pulmonary Practice Questions
This blog is intended for students in the health sciences and other students with an interest in cardiovascular, pulmonary and renal physiology and pathophysiology. It is a compilation of original contributions as well as notes I have taken during lectures on these topics and clinical lectures. At the bottom of each post is a box for comments that you are invited to use. Steve Wood, PhD, swood60@gmail.com teaching website: http://www.cvpulmrenal.com
Saturday, April 1, 2017
Friday, March 31, 2017
Alveolar-arterial PO2 difference (A-a)PO2 breathing 100% oxygen
Would the alveolar-arterial PO2 difference (A-a)PO2 be normal in a healthy person breathing 100% oxygen; i.e., would alveolar and arterial PO2 both increase by the same amount?
No, the (A-a)PO2 will be greatly increased in healthy lungs breathing 100% O2.
The figure below shows inspired to venous blood partial pressures during O2 breathing at 1 ATA (100% O2 at sea level). In this example, it is assumed that all nitrogen, argon and other trace gasses have been washed out of the system. During O2 breathing, the ventilation/perfusion inequalities in lung have a much greater impact on PaO2 than during air breathing. Under optimal conditions during O2 breathing at 1 ATA, PaO2 would be about 500 mmHg while alveolar PO2 is about 663 mm Hg. (PAO2 = (760 - 47) - 40/.8 = 663). As blood moves through tissue, the same 4.5 mL O2/dL blood is extracted, and PO2 falls to 57 mmHg in venous blood.
A look at the oxyhemoglobin dissociation curve helps explain why the (A-a)PO2 difference is so high. Because of the flat upper portion of the curve, a small drop in O2 content due to normal shunts and low V/Q cause a large drop in PO₂ (from PAO₂ = 663 to PaO₂ = 500 mm Hg.
Is the sum of partial pressures of gases in blood equal to total atmospheric pressure?
Is the sum of partial pressures of gases in blood equal to total atmospheric pressure?
Not necessarily. This is true for alveolar gas pressures but not for blood. For practical purposes, liquids are incompressible and do not respond to changes in ambient pressure. Because of this, the sum of gas partial pressures in a liquid can be less than ambient pressure. Liquids such as blood and other body tissues will equilibrate only with the gas partial pressures to which they are exposed.
On the alveolar side of the alveolar membrane, the total partial pressures must equal ambient pressure. However, on the liquid side of the membrane, the total partial pressures can be less, and in some areas may be quite a bit less than ambient pressure. The partial pressure that a gas exerts in a liquid depends on the temperature, the solubility of the gas in the liquid and the amount of gas present. Thus, if the amount of gas present and the temperature remain constant, the partial pressure of the gas in a tissue is fixed. If one gas is removed from a tissue, the remaining gases do not expand to fill the partial pressure vacated by the gas that was removed. The figure below shows total partial pressures for air breathing at 1 ATA from inspired gas to venous blood. Because of the decline in PO2 from alveoli to arterial blood, the total gas partial pressure in arterial blood during air breathing at 1 ATA is 752 mmHg, less than ambient pressure (760 mmHg). If PaO2 is lower than 95 mmHg (assumed in this example), then the total partial pressure in arterial blood will be less.
Sunday, March 26, 2017
Emphysema - what the lung looks like
Emphysema
Normal Lung Emphysema
Normal Lung Smoker's Lung
Emphysema vs Chronic bronchitis
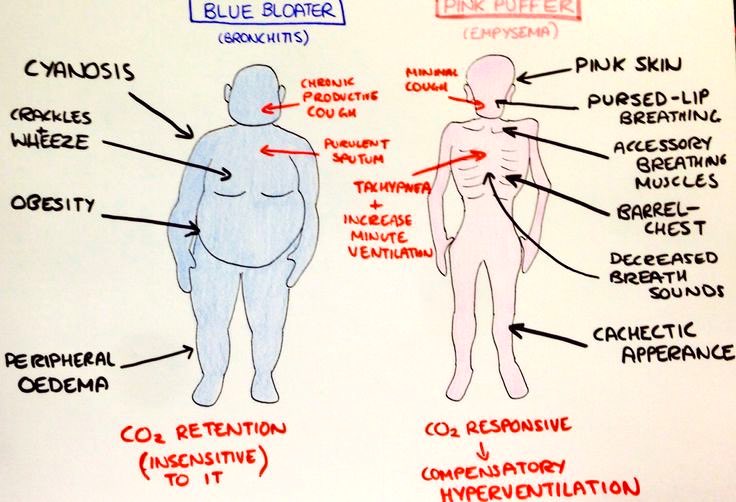
Pink puffers: emphysema
destruction of the airways distal to the terminal bronchioles--which also includes the gradual destruction of the pulmonary capillary bed and thus decreased inability to oxygenate the blood. So, not only is there less surface area for gas exchange, there is also less vascular bed for gas exchange--but less ventilation-perfusion mismatch than blue bloaters (hence: pink if compared to bronchitis). The body then has to compensate by hyperventilation (the "puffer" part). Some of the pink appearance may be due to the work (use of neck and chest muscles) these folks put into just drawing a breath.
Blue bloater: chronic bronchitis.
caused by excessive mucus production with airway obstruction resulting from hyperplasia of mucus-producing glands, goblet cell metaplasia, and chronic inflammation around bronchi. Unlike emphysema, the pulmonary capillary bed is undamaged. Instead, the body responds to the increased obstruction by decreasing ventilation and increasing cardiac output. There is severe ventilation to perfusion mismatch leading to hypoxemia and polycythemia.
Because of increasing obstruction, residual lung volume gradually increases (the "bloating" part). They are hypoxemic/cyanotic because they actually have worse hypoxemia than pink puffers
Subscribe to:
Comments (Atom)




